Quality Improvement
Quality Measures
Our dashboards provide concise information and are also highly interactive for administrators who like to dive deeper into the data. This data also is HIPAA compliant to secure Protected Health Information (PHI). Administrators can look at measures comparable to state and national protocols to determine performance improvement projects. Administrators can focus on a process to view and develop corrective action plans. Our Summary of Outcomes provides a conclusion of YTD information comparing agency outcomes against state and national level scores.
Clinical Outcome Measures (including VBP measures)
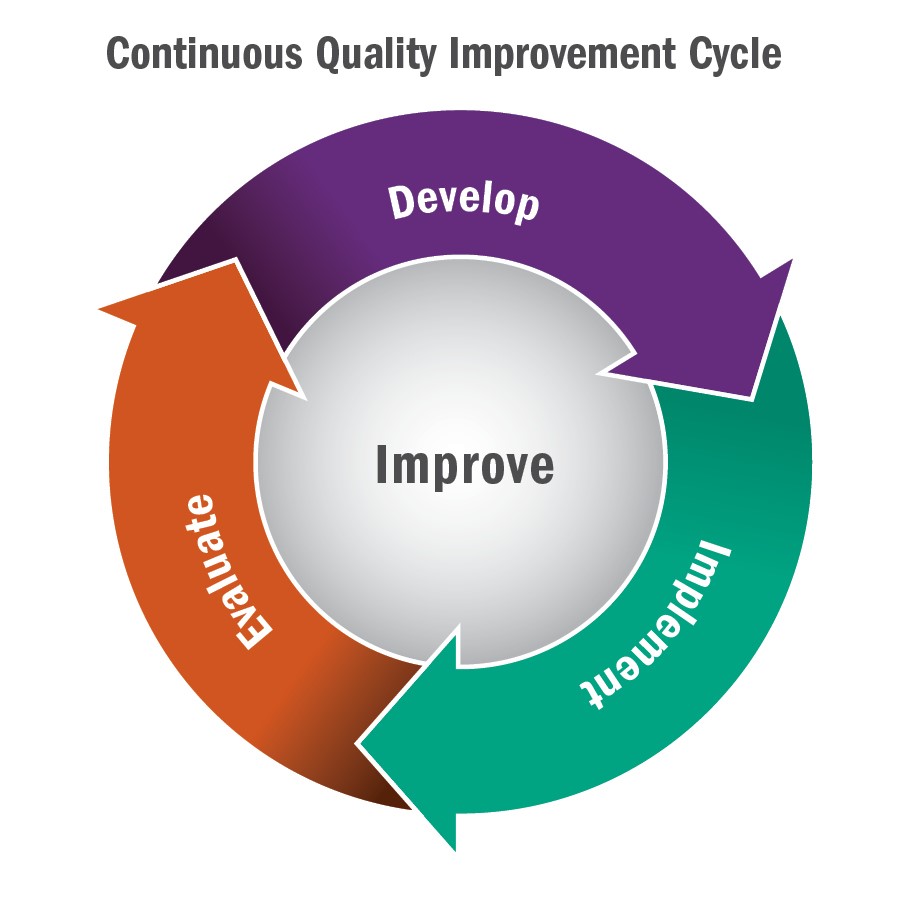
HealthWare’s analysis of diagnostic trends, and other information of a specific measure, will help determine an agency’s Quality Assessment and Performance Improvement (QAPI) project focus. Once a measure is picked and action plan is in place, use the dashboard to view the measure over time and evaluate the plan’s performance and progress. Our report displays patients who have been discharged, readmitted, or retained for chart and care plan review and can be used to develop a corrective action plan. An example: An administrator can review care plans for patients, who have experienced a decline in ambulation, to determine their reason for this decline. Discovering scoring inconsistencies between clinicians is an essential component of this measurement. HealthWare also provides the Disease Section and Chapter including secondary and tertiary diagnostic information. Our trending page can assess other relevant patient factors such as living situation, ambulation, vision, and disease progression. We provide the ability to manage the entire QAPI program and then measure its progress. HealthWare continuously evaluates agency data, for consistency and quality improvement purposes, before submission to CMS for the Star Ratings process. Bottom Line: HealthWare’s over 33 years of experience will give the agency an efficient and comprehensive collection, analyzation, and measurement of data. Our Microsoft partnership enhances our leading-edge technology. Our tools provide an interactive experience to help agencies develop their own specific QAPI programs.
Non- Clinical Measures
We also report on non-clinical measures such as timely initiation of care, multiple admissions, diagnosis changes and more.
Risk Assessment
Using our predictive rules engine, at the start of care, will predict the outcome performance for the episode, on quality measures such as ambulation, pain, transfers, and ADLs. This process offers an insight to review and change procedures that will affect outcomes over time. HealthWare Quality Outcomes subscribers meet all compliance factors for a data driven quality program indicated in the Conditions of Participation.